The Beginners Guide to Understanding Cardiology
by David Peck, EMT-P STAR Ambulance Service
Contributing writer for Public Safety Degrees
Introduction
Philosophically you could argue that the heart is the single most important organ in your body. Someone could even have no brain activity and be classified as "living." Declarations of death only come after a heart has ceased beating entirely. As a result, approximately 75 percent of all drugs that ambulances carry affect the heart in some way.
It seems that every few weeks or so I have a curious patient who catches a glance at the screen of the cardiac monitor and inevitably asks, "So what do all those bumps and spikes mean?" Depending on how much they want to know; they may have just asked the wrong medic the wrong question. I've given countless 45 minute "courses" in cardiology to people of from all walks of life during transports from rural hospitals to larger specialty facilities. Now these patients weren't qualified to perform their own cardiac catheterizations, but they did understand what all those "bumps and spikes" meant and why they are important. I have now put this "course" to paper in hopes of better educating healthcare workers and those who wish to know more about perhaps the most important part of anyone's body.
Two Equally Important Cardiac Systems
It is easiest to think of the heart as having two separate, but equally important systems: Mechanical and Electrical. Similar to a car engine, however in this analogy your car's battery is built into the engine and gasoline is actually blood.
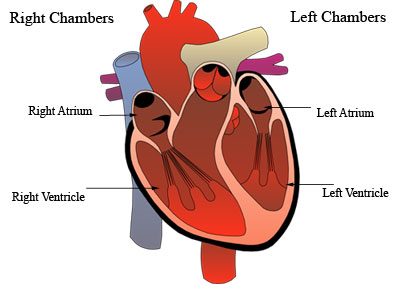
The moving parts of your heart are all classified as mechanical. They consist of 4 blood filled chambers and valves connecting these chambers to blood vessels. The chambers are known as the Left and Right Atria (the top half of you heart) and the Left and Right Ventricles (the bottom half).
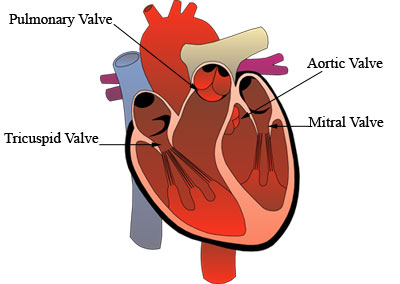
The valves that open and shut allowing blood to pass from chamber to chamber and into vessels are known as: the Tricuspid Valve, the Pulmonary Valve, the Mitral Valve, and finally the Aortic Valve.
Blood is pumped through your heart in a very specific pattern, and any deviation of this pattern is certainly a problem. Tracing a drop of blood through the heart and back out to your body happens in these chronological steps.
- De-oxygenated blood returns from your veins to your Right Atrium
- Blood is then pumped through the Tricuspid Valve to the Right Ventricle
- Blood is pumped out of the heart to the lungs via the Pulmonary Valve; where blood is then re-oxygenated
- Oxygen rich blood returns from the lungs to the Left Atrium
- Blood is then pumped through the Mitral Valve to the Left Ventricle
- Blood is finally pumped through the Aortic Valve and out the body You can feel this step every time you feel a pulse)
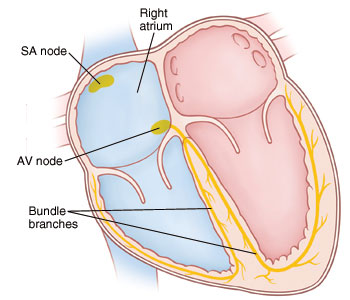
That sums up the mechanical aspect of the heart, but the catch is that none of it works without electrical power. The heart has its own electrical power plant, backup power plants, and electrical lines running through it. The primary powerhouse is located in the top of your heart and is known as the Sino-Atrial node (SA node). It generates an electrical impulse normally ranging from 60 to 100 beats per minute. The impulse travels down through the Atrias causing a contraction to the middle of the heart known as the Atrio-Ventricular Node/Junction (AV node). This node acts as a secondary backup plant should the first begin to fail and has intrinsic firing rate of 40 to 60 beats per minute. The original electrical impulse continues down into the Ventricles where it splits into the Left and Right Bundle Branches and finally to an endless network of wires known as the Purkinje Fibers causing a Ventricular contraction. These fibers are also the hearts last resort should the SA and AV node fail. Their intrinsic firing rate is a paltry 20 to 40 beats per minute. That is hardly enough to live on for any length of time.
Electrocardiograms

In 1924 William Einthoven won the Nobel Prize for Physiology for his research and creation of the Electrocardiogram (ECG). The bulky machine pictured, over the past 80 plus years, has been reduced to much smaller, portable machines that in addition to cardiac monitoring can perform a vast array of other functions. The buckets of saltwater that his arms and leg are in have been shrunk to small stickers with a dab of gel, that are placed at key points on the body.
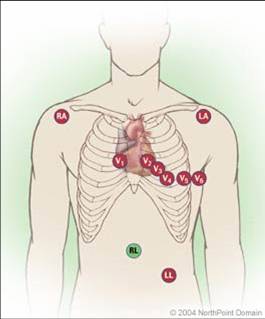
However for all the change the purpose remains the same. The ECG monitors the electrical activity of the heart, makes a tracing, and allows for real time interpretation of a "rhythm." It is important to understand the machine in order to understand the rhythm. Pictured here is traditional 12-lead placement for an ECG. Each one of the electrodes act as an "eye" allowing you visualize different angles of the heart. The limb leads consist of RA=Right Arm, LA=Left Arm, RL=Right Leg, LL=Left Leg. The precordial leads consist of V1 through V6.
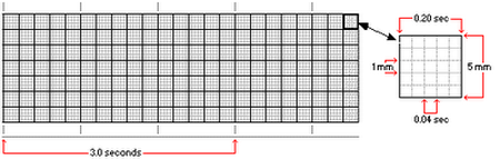
ECG tracings print out on various colors and types of paper, but all will have the same measurements. Notice that ECG paper is a grid of boxes going vertically and horizontally. Vertically the boxes represent amplitude; horizontally the boxes are a representation of time.
Specifically one small box horizontally equals 0.04 seconds. Five of these small boxes make up a larger box which is equal to 0.2 seconds. Therefore five of the larger boxes are equal to exactly one second of time. This is important in order to evaluate not only how fast the heart is beating, but also to measure how fast each part of the heart is working.
Normal Waveforms
The image below is a representation of a singular, normal heart beat. Each waveform and deflection is labeled with a letter. But what they actually represent are contractions of the heart. The first small vertical bump is known as the "P-wave." This occurs when the SA node generates an electrical impulse causing the Atrias (the top) of the heart to contract. That impulse travels down through the heart to the Ventricles. A normal time for this to happen should be between 0.12-0.20 seconds. The P-wave and the space between it and next positive (upward) deflection are known as the PR interval.
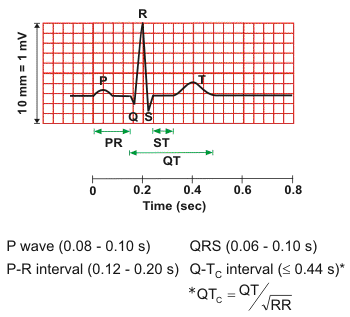
Should there be a negative (downward) deflection before a positive deflection it is known as a Q-wave. Not all ECGs will have a Q-wave. The first positive deflection is known as an R-wave, which will be immediately followed by another negative deflection known as an S-wave. All together this is known as a QRS complex. It is the visual representation of the larger, stronger Ventricles contracting. Each QRS complex should have a corresponding pulse with it. The normal length of time for a QRS complex to complete should be 0.08-0.10 seconds.
Next is the segment of line between the S-wave and the beginning of the T-wave. This is known as the ST segment. Ideally this segment should be vertically equal as the isometric line (line before the P-wave and after the T-wave). Should this segment be lower than or higher than the isometric line by more then two small boxes then potentially a critical problem exists.
Finally the last wave form in the sequence is a larger vertical wave known as a T-wave. This is the representation of the Ventricles re-polarizing (filling back up with blood). You may be asking when the Atrias re-polarize. The answer is that atrial re-polarization occurs simultaneously during ventricular contraction. However since ventricular contraction puts out a much stronger electrical impulse, a total eclipse of an atrial re-polarization waveform occurs.
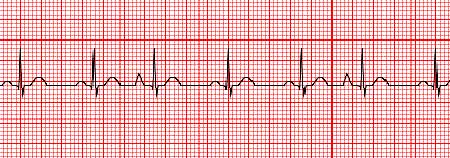
Sinus Rhythms
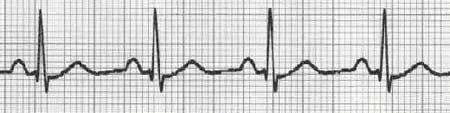
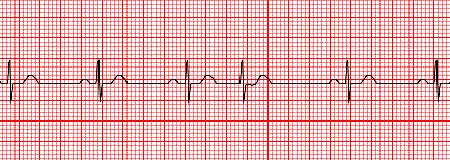
A healthy heart will beat in a sinus rhythm. The term sinus rhythm is derived from Sino-Atrial node. This is because in order to have a sinus rhythm, the rhythm must originate in the SA node. It absolutely WILL have a P-wave. This is the first rule in determining a sinus rhythm. It will beat between 60-100bpm. Slower than 60bpm and the rhythm is known as Sinus Bradycardia. Faster than 100bpm it is known as Sinus Tachycardia.
Normal Sinus Rythm
Sinus Bradycardia
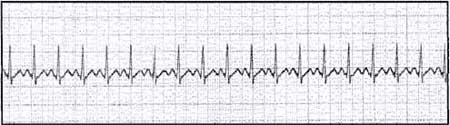
Sinus Tachycardia
Atrial Rhythms
Some rhythms originate in the Atrias, but not in SA node. Rather somewhere along the inter-nodal electrical tract between the SA node and the AV node. Two common rhythms are known as Atrial Fibrillation (A-fib) and Atrial Flutter (A-flutter).
A-fib is a common dysrhythmia that occurs as a result of the Atrias quivering instead of contracting. This results in frequent, irregular impulses being sent through the AV node to the ventricles. Often this will result in a rapid ventricular response (RVR) and will need emergency care. A-fib has a few unique characteristics to identify on an ECG. A-fib will be quite irregular in ventricular contraction. Often times just by feeling a patient's pulse will reveal A-fib prior to ECG placement. Also A-fib will lack a definitive P-wave prior to each QRS complex. Occasionally small quivering lines will occur between QRS complexes.
Atrial Fibrillation
A-flutter is very similar in nature to that of A-fib. Instead of merely quivering, instead the Atria are contracting very rapidly. This can also result in RVR. Additionally A-flutter can be regular or irregular. Before each QRS complex will be at least one flutter wave, sometimes many more. A flutter wave is similar to a P-wave except that often times there will be a varying amount of them.
Atrial Flutter with a 3 flutter wave to 1 QRS conduction

Atrial Flutter with a varying flutter wave conduction
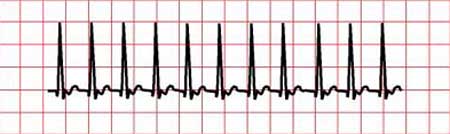
Supraventricular Tachycardia, a Cyclical Problem
A common dysrhythmia that afflicts certain people is Supraventicular Tachycardia (SVT). This rhythm originates either in the SA node, or near it, hence the name "Supra" meaning "above" the ventricles. When the electrical impulse is generated and flows down the normal electrical pathway, an additional pathway is found that circles back around to the top of the heart. So simultaneously each impulse that generates a heartbeat also reactivates the heart causing yet another heartbeat. This cycle continues inevitably speeding the heart rate to an intolerable level causing chest pain and shortness of breath. Often this rate can be in excess of 160bpm, obscuring the P-wave from an ECG. SVT will have a narrow QRS complex and will be regular. If the QRS is wide the ECG evaluator should suspect Ventricular Tachycardia, and should the rhythm be irregular A-fib with RVR should be suspected.
Supraventricular Tachycardia
Junctional Rhythms
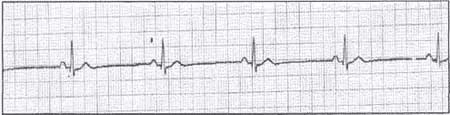
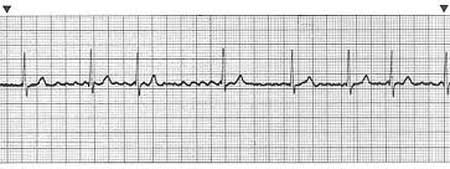
What were to happen if the SA node failed? The AV node is located at the junction of the Atrias and the Ventricles; it is also the first of two backup pacemakers for the heart. Unsurprisingly, the rhythms originating from the AV node are known as Junctional Rhythms. The intrinsic firing rate is between 40-60bpm. Just like Sinus rhythms, if the rate is slower than the intrinsic parameters it is known as bradycardia. Conversely, faster than intrinsic parameters is known as Accelerated Junctional. Perhaps the most distinguishable feature of Junctional Rhythms is the P-wave. Junctional Rhythms will have either an inverted P-wave or lack one all together. Additionally the P-wave may occur before or after the QRS complex The QRS complex will be also be narrow to slightly wider than that of Sinus Rhythms.
Junctional Rhythm with Inverted P-wave

Accelerated Junctional Rhythm with no P-wave

Ventricular Rhythms
There are a few Ventricular Rhythms: Idioventricular, Ventricular Tachycardia (V-tach), and Ventricular Fibrillation (V-fib). None of these rhythms are capable of sustaining life for any great length of time. Ventricular Rhythms originate in the final backup pacemaker for the heart, the bundle branches/purkinje fibers. Intrinsic firing rates of these rhythms vary wildly. Idioventricular Rhythm's intrinsic rate is 20-40bpm. Just like Junctional, if the rate is faster than the intrinsic parameters it is known as Accelerated Idioventricular. Slower than the intrinsic parameters is known as bradycardia. Idioventricular will have no P-wave as the atrias are not contracting. The QRS complex will be very wide and regular. This is the rhythm of a heart with a dying electrical system.
Idioventricular Rhythm

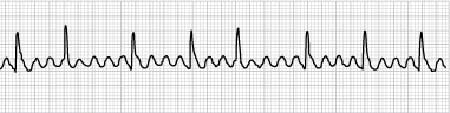
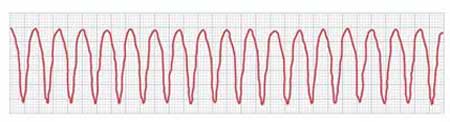
V-tach is a very dangerous rhythm. It may or may not have an associated pulse. V-tach causes the ventricles to contract at extremely fast rates, generally 150-300bpm. With contractions occurring so fast it is possible that the ventricles will not fill with blood to expel to the body resulting in no pulse. In this event, the need for CPR and defibrillation is most urgent. It is possible that a patient with stable vital signs will present with V-tach. Emergency action is still needed required. V-tach will appear with no P-wave or T-wave. The QRS will be very wide and regular, resembling a saw blade.
Ventricular Tachycardia
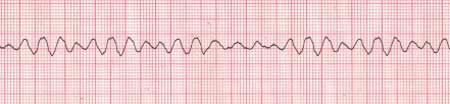
V-fib is a cardiac arrest rhythm. It will NEVER have a pulse associated with it as the ventricles are quivering or "fibrillating," not contracting. Survival from this lethal rhythm requires immediate CPR, defibrillation, and ACLS procedures. V-fib is characterized by chaotic indistinguishable waveforms. The waveforms will range from large/coarse to small/fine. V-fib will not feature a P-wave, QRS complex, or T-wave.
Ventricular Fibrillation
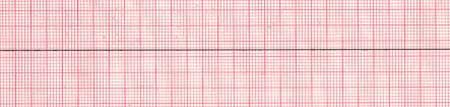
Asystole
In medicine, adding the "A" prefix to a word generally means "without". So, it stands to reason that "Asystole" would mean "without systolic function". A rhythm that needs no introduction as it is featured in several films and television shows each year is Asystole. Asystole is simply when the heart is no longer generating any electrical impulses. It is represented by a simple flat line on the ECG. Occasionally a wide, pulseless wave form will appear at random, known as an agonal complex. CPR and ACLS medication are required for a chance at survival.
Asystole
Escape Beats
There are three types of escape beats. They are Premature Atrial Contractions (PAC's), Premature Junctional Contractions (PJC's), and Premature Ventricular Contractions (PVC's). Escape beats are extra waveforms outside of the patients underlying rhythm. How they look and are classified is dependent on where the beat originates from along the electrical pathway. PAC's as their name implies originate in the atrias. They will look just like a regular sinus beats, including a P-Wave, except they will occur earlier than normal in the patient's regular rate. This will cause the rhythm to look irregular. PAC's will have a pulse and are generally harmless.
Sinus Rhythm with PAC's
PJC's originate in and around the AV node. It will appear earlier than the next scheduled beat depending on the patient's heart rate, causing the rhythm to appear irregular. Just like a Junctional Rhythm, a PJC will either have an inverted P-wave or lack one all together. Additionally PJC's will also have a pulse associated with them, therefore generally harmless.
Sinus Rhythm with a PJC
Premature Ventricular Contractions (PVCs)
PVC's originate in ventricles along the bundle branches/purkinje fibers. They lack a P-wave and the QRS complexes will be wide and abnormal in appearance. PVC's can originate on a relatively long path; therefore PVC's can look quite different from one another. Having PVC's generating from different locations along the bundle branches are known as "multi-focal." Conversely to other escape beats, PVC's traditionally do not have pulse associated with them. This is because the ventricles are not given time to refill with blood from the atrias before they contract again. Therefore singular PVC's are not that threatening and it is possible that a patient may not even notice one. However frequent PVC's can cause a patient to experience dizziness, nausea and shortness of breath. If a patient were to begin experience extended runs of PVC's consecutively, their blood pressure would drop and a need for emergency care would arise.
Sinus Rhythm with Multi-focal PVC's

Conclusion
This article merely scratches the surface of cardiology and ECG interpretation. Additionally, the American Heart Association's course "ACLS" is a valuable resource for those looking for the clinical implications and recommended treatments of ECG dysrhythmias. Hopefully this article has helped shed light on the meaning of all those "bumps and spikes."
If you like this article, please also read A Guide to STEMIs: Basic 12 lead diagnosis and treatment


