A Guide to STEMIs: Basic 12 lead diagnosis and treatment
by David Peck, EMT-P STAR Ambulance Service
Contributing writer for Public Safety Degrees
If you have worked in emergency medicine for even just a short amount of time, chances are you have heard the term "STEMI" (pronounced stem-ee). If by some strange miracle you have not, just give it time as the rapid recognition and treatment of STEMI's has become a major focus all around the country. So what exactly is a STEMI? The term STEMI is actually an acronym for (ST segment Elevated Myocardial Infarction). Ultimately in laymen's terms, this is a very grave heart attack that a victim's survivability is dependent upon quick and aggressive treatment from all care providers, beginning with First Responders and all the way to the cardiologist.
Recognition of a STEMI requires some advanced prerequisite knowledge of ECG's and cardiology. If ECG assessment is a new subject for the reader or perhaps the reader is just a little rusty, it recommended that you read The Beginner's Guide to Cardiology.
The Importance of the ST Segment
The ST segment refers to area of ECG beginning with the end of the "S-wave" and ending with the start of the "T-wave."
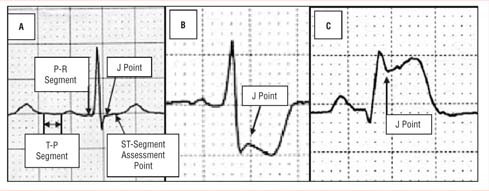
True measurement of the ST segment begins at the "J-point" after the S-wave. The J-point is the initial point where line of the ECG ceases having a vertical or diagonal angle and flattens out to become more straight leading to the T-wave. Ideally the beginning of the J-point will be vertically equal to the isometric line as seen in figure A below. When the J-point of the ST segment is below the isometric line it referred to as depressed as seen in figure B. Should the J-point begin higher than the isometric line as seen in figure C, it is referred to as elevated. Changes to the ST segment of either depression or elevation must be greater than 2mm (vertically two small boxes).
When the ST segment is depressed this indicates myocardial ischemia (a lack of oxygen to the heart muscle itself). Additionally ECG leads showing ST depression could be the result of reciprocal (mirrored) changes of other leads showing ST elevation. Reciprocal changes frequently occur in an area opposite of elevation and can be a great clue to healthcare providers that ST elevation exists somewhere else in the heart. Possibly even on other areas of the heart such as the posterior wall. This is just one of many reasons why it is important to obtain a full 12-lead ECG for all patients suspected of having cardiac related complaints.
ST elevation is an indication myocardial injury. This means that actual heart muscle tissue death has occurred due to a blockage of a coronary artery that provides newly oxygenated blood. Blockages are normally caused by either excessive plaque buildup or a lodged blood clot. The tissue damage will continue to spread until the blockage or blockages are opened via angioplasty or thrombolytic (clot buster) medication. Hence the phrase "Time is Muscle."
12 Lead Placement and Interpretation
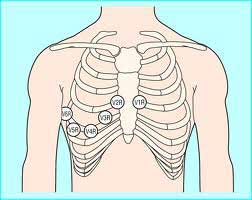
When assessing a potential cardiac patient it is important to obtain a 12 lead ECG as soon as possible. A traditional 12 lead ECG looks at four planes of the heart. The Inferior (the bottom), the Anterior (the front), the Lateral (outside wall closest to the patients left arm), and finally the Septal (inside wall closest to the sternum). Obtaining a 12 lead ECG can allow a technician to locate the area of the heart showing elevation, which will allow a cardiologist to more rapidly intervene in opening a blockage. Below is a picture of the traditional 12 leads of an ECG and what wall they look at respectively. Notice that aVR does not look at a heart wall. The lead aVR (augment Voltage Right) actually looks at the great vessels above the heart such as the aorta and the superior vena cava.
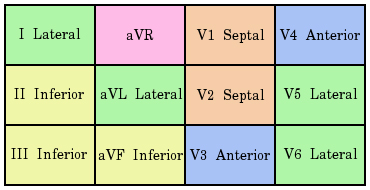
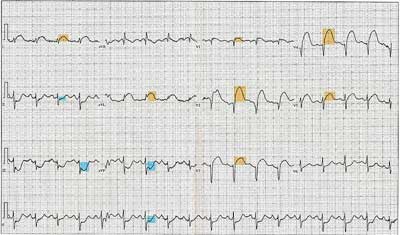
Another qualification for a STEMI is that there must be at least two leads of the same wall or contiguous (connected) walls that are elevated. So for instance should leads II and III be elevated this would be known as an Inferior STEMI. Or if leads V4 and V5 had elevation this would be known as an Antero-lateral STEMI. Note some the examples here.
Inferior STEMI
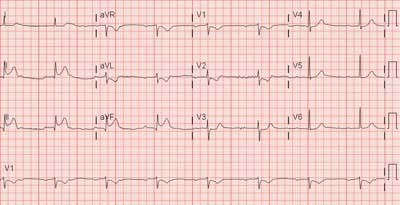
Septal STEMI

Septal-Anterior-Lateral STEMI (note the reciprocal changes to the inferior leads in blue)
It is important to know that occasionally additional types of 12 lead ECGs may be required to locate possible elevation. Not all STEMI's occur within the traditional four walls. It may be pertinent to obtain a "Right Sided ECG" and or a "Posterior ECG." Performing a Right Sided ECG allows for a better view of the Right Ventricle and Atrium. This can be obtained by placing the pre-cordial leads (V1-V6) along the right side of the chest in the same anatomical intercostal locations as their traditional placement. Now these leads will be known as V1R- V6R and should be documented as such on all printed ECG's.
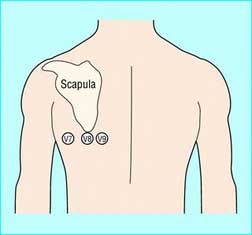
Perhaps the most forgotten area of the heart is the posterior wall. It is rare to find any EMS providers or even non-cardiac specialty ED's performing assessments of the posterior wall. However performing a Posterior ECG could be lifesaving if it discovers a STEMI that would otherwise go untreated or at best be treated much later after considerably more damage is done. Reciprocal changes are often the best indicator for the need for a Posterior ECG. Cardiac patients who present with ST depression in multiple leads, commonly the anterior leads, yet have no elevation noted in a traditional 12 lead would be prime candidates to perform a Posterior ECG.
A Posterior ECG is performed by placing leads V4 - V6 on the back. The location of each lead is the same as if you drew an imaginary line from each leads original placement on the front of the chest to the back. This should be just below the shoulder blade on the left side of the patient's back. Now these leads will be known as V7-V8 and should be documented on all printed ECG's. It should be noted that Posterior ECG voltage will be reduced due to the increased distance from the heart as well as the left lung. This can often make recognition of ST elevation more difficult to identify.
Pre-hospital Treatment of STEMI
In conclusion, no matter the STEMI location, it is a serious life threatening emergency and rapid assessment and treatment can drastically impact the quality of life for the patient. Statistically, Inferior STEMI's are the most common. They making up between 40-50 percent of all STEMI's. Of those, about 80 percent of the blockages are located in the right coronary artery. The most lethal STEMI's are those located in the anterior wall and have a mortality rate of 27 percent, earning them the ominous nickname "the widow maker." It remains vital that all providers "treat the patient and not the monitor," as there are some differential diagnosis when presented with ST elevation including pericarditis and aortic dissection.
Treatment of a STEMI patient can begin before the actual recognition of one occurs. Basic Life Support (BLS) providers can begin appropriate care by administering high flow O2, assessing vital signs and administering/assisting with oral aspirin and sublingual nitroglycerin depending on local protocols. When full ECG trained providers are available, rapid recognition should become the primary goal. While ACLS medications and interventions are important, ultimately the only cure to any STEMI is the eradication of the blockage and reperfusion of the damaged heart tissue. Pre-hospital providers should become familiarized with locations of cardiac catheterization laboratories. Studies have shown that in many scenarios, the total patient outcome/recovery is better when a patient is transported to cath labs and bypassing closer hospitals without them. As a result many rural hospitals and EMS services are designing new sets of protocols for the special treatment and transportation of STEMI patients.

